Summarized by : Dr. Hani Alhebshi
An orthodontist can face cases of dental trauma at his\her practice from time to time. These traumatic injuries differ in their types, severity and management.
This is a summary of the most common situations of dental traumas and their management. This is based on two fantastic articles I strongly encourage to read.
Assessment and diagnosis of dental trauma
a comprehensive dental history which includes : asking about previous episodes of dental trauma or treatment.
a comprehensive clinical and radiographic assessment is essential prior to commencing orthodontic treatment and should include:
1. Hard tissue assessment
a. Crown color assessment:
-
- Dark hue might indicate loss of pulp vitality.
- Yellow colour might indicate pulp canal obliteration
- Pink colour might indicate internal resorption.
b. Transillumination assessment can reveal enamel infraction lines and colour changes in traumatised teeth.
c. Assessment of tooth mobility in both horizontal and vertical directions.
d. Percussion tests:
- Tenderness to touching or tapping a tooth is suggestive of PDL damage.
- High metallic percussion note is often diagnostic of ankylosis.
- Dull percussion note may be suggestive of a root fracture.
2. Soft tissue assessment:
a. Sinus tracts or swellings indicate peri-radicular infection.
b. Palpation over the tooth apex for tenderness as it might indicate a periapical infection.
3. Radiographic assessment:
-
- Two radiographs taken at different angulations are usually required to detect a root fracture.
- Radiographs can detect any root resorption or pulp canal obliteration due to previous trauma.
- It is often very helpful if periapical radiographs of traumatized central incisors include both the injured tooth and its uninjured counterpart for direct comparison.
4. Sensibility tests:
-
- Sensibility tests should be considered in association with other clinical and radiographic findings but not in isolation.
- Electric pulp testing (EPT) is the most useful test to assess the neurovascular supply to the pulp of a traumatised tooth. The electrode should be placed as close to the incisal edge as possible to avoid contact with the gingival tissues and hence obtaining false-positive results.
- The use of the EPT in developing teeth is unreliable.
- Laser Doppler flowmetry is the only objective measure of pulp vitality available and is shown to be reliable in assessing pulp blood supply.
Prevention of dental trauma
- Interceptive treatment and use of sports mouth guards.
- Prominent incisor position and inadequate lip coverage were found to be the most consistent risk factors related to dental trauma and suggested that early interceptive treatment should be considered to reduce the risk of dental trauma.
- Early mixed dentition orthodontic treatment for children with an overjet greater than 9 mm (IOTN 5a) could reduce the risk of damage to incisors.
Effects of orthodontic tooth movement on traumatized teeth
Pulp vitality
With the evidence currently available it is not possible to say whether orthodontic tooth movement of traumatized teeth increases the risk of pulp necrosis above that of uninjured teeth undergoing tooth movement.
Root resorption
There are three main types of root resorption:
surface resorption, inflammatory resorption and replacement resorption ( Ankylosis ).
Table .. Observation periods before re-commencing orthodontic treatment
|
Condition |
Conditions / cause / Severity |
Observation Period before commencing Orthodontic movement / Management |
|
|
|
|
|
Trauma
|
Minor |
3 months |
|
Moderate to severe |
1 year .. if no ankylosis |
|
|
|
|
|
|
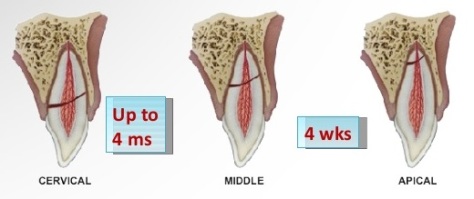
Root Fracture depends on level of the fracture whether at : Apical/midroot , Cervical.
|
2 years or 1 year if no complications. |
|
|
Apical/midroot |
Splint for 4 weeks then do endo. |
|
|
Cervical root fracture |
Splint for 4 months then do endo. |
|
|
Immature Root |
6 months, 1 year then 2 years |
|
|
|
|
|
|
A Tooth with root canal treatment (RCT) Depends on the cause and stage of root development |
if RCT due to caries |
start treatment immediately. |
|
RCT due to inflammation |
1 year |
|
|
|
If no Root resorption |
Place Gutta Percha |
|
Closed Root / asymptomatic |
CaOH for 4 weeks then change it to Gutta percha |
|
|
If there is root resorption |
CaOH for 12 weeks to promote cementum formation. Then place Gutta percha. |
|
|
|
|
|
|
Intrusion of Maxillary incisor |
Open Apex |
|
|
Mild < 3 mm |
Allow spontaneous eruption. |
|
|
|
Moderate 3-6 mm |
Allow spontaneous eruption or reposition within 2 weeks. If not erupted,reposition orthodontically |
|
Severe > 6 mm |
Surgical repositioning |
|
|
Closed Apex |
||
|
Mild < 3 mm |
Allow spontaneous eruption or reposition within 2 weeks. If not erupted,reposition orthodontically |
|
|
Moderate 3-6 mm |
reposition within 2 weeks to allow RCT orthodontically |
|
|
Severe > 6 mm |
Surgical repositioning |
|
|
|
|
|
|
Ankylosis
|
If tooth doesn’t move in 8 weeks , it might indicate ankylosis. |
Build up – Decoronation or Extraction. |
|
|
|
|
|
Avulsion |
Depends on extraoral time and extra-alveolar time , 90 minutes extra-alveolar time ( dry / wet ).
90% of ankyloses if tooth repositioned beyond these times. |
should be replanted as soon as possible, unless contraindicated for reasons such as medical history or patient cooperation. |
|
|
|
|
|
Trauma During orthodontic treatment Depends on which stage trauma has occurred and which arch wire was there at time of trauma. Initial – Middle – End stage. |
Initial Stage
|
Usually it reposition automatically. |
|
|
Middle Stage |
Minor displacement => reposition the bracket and place NITI wire to normalize. Severe displacement => Surgical repositioning and place NITI wire. |
|
End stage |
SS usually has a protective mechanism against tooth displacement.
|
|
|
|
|
|
|
Autotransplantation |
||
|
Best teeth to autotransplant are L4 , L5 and U5 |
Indications of autotransplantation => |
1. Excellent Oral hygiene. 2. Cooperative and motivated patient. 3. Treatment plan has extraction strategy of one or more of the proposed teeth (L4,L5,U5). |
|
|
If Immature root |
1 month , 3 months and 1 year. (after 6 months PDL healing) |
|
|
If Mature root |
Splint 10 – 14 days Pulp extirpation at day of splint removal. |
Increased Risk of Root Resorption depend on :
- The length of orthodontic treatment time.
- Root morphology, (blunt or pipette shaped roots is significantly greater).
- Force applied .
- Previous dental trauma.
- It has been recommended that radiographs are taken three months after the commencement of orthodontic treatment in teeth with blunt or pipette shaped apices.
- Previous trauma may be predictive of an increased risk of root resorption during orthodontic treatment.
Radiographic monitoring of traumatized teeth or teeth with pre-treatment root resorption
Current recommendations for radiographic assessment of traumatized teeth or teeth showing signs of pretreatment root resorption, during orthodontic treatment :
1. Baseline periapical radiographs or an upper standard occlusal radiograph.
2. Repeated views six to nine months into treatment.
-
-
- If minor root resorption is noted and a decision made to continue with orthodontic treatment, further radiographs should be taken after three months.
- If severe root resorption a rest period of three months is recommended prior to recommencing orthodontic treatment.
- a risk of permanent tooth mobility has been shown to occur if the total root length is less than or equal to 9 mm.
- This risk is reduced if more than 9 mm of tooth root remains in the presence of a healthy periodontium.
-
Orthodontic tooth movement in root treated teeth
From the available evidence it can be concluded that there is no significant difference in the root resorption of endodontically treated teeth when compared to vital teeth subjected to the same orthodontic forces.
Orthodontic management of root filled Teeth
Choice of root-filling material
The European Society of Endodontology published quality assurance guidelines stating that endodontic treatment can be considered successful one year post obturation when there is absence of pain or swelling, no sinus tract, no loss of function and radiographic evidence of a normal periodontal ligament space around the tooth.
- A definitively obturated (Gutta percha ) and coronally sealed root treated tooth would appear to be at no greater risk of root resorption during tooth movement than one in which an interim dressing is maintained.
- When there is established external inflammatory root resorption, long-term calcium hydroxide treatment (12 weeks) is significantly more effective than short-term treatment (1 week application prior to obturation) in promoting root surface healing with new cementum.
- A definitive obturation of a non-vital tooth must be completed at the earliest opportunity prior to orthodontic tooth movement, in most cases
Observation periods following endodontic treatment prior to orthodontic tooth movement
Please See the table above.
Where there has been extensive bone loss , tooth movement should be delayed until there are clinical and radiographic signs of some healing and an interval of at least six months has been suggested.
Force levels and mechanics for root-filled teeth
Normal force levels (net force of 50–100 g on a central incisor for bodily movement) can be used, providing the periodontal ligament is healthy.
References :
- Semin Orthod 2015; 21:59–70. Upper incisor trauma and the orthodontic
patient—Principles of management by Monty Singh Duggal et al. - Journal of Orthodontics, Vol. 35, 2008, 68–78 , Dental trauma: an overview of its
influence on the management of orthodontic treatment. Part 1 , by Susan A. Kindelan et al.

Thank you so much .for that interested subject
في الاثنين، ١٣ أبريل ٢٠٢٠ ٤:٥٠ م Saudi Board Ortho Club كتب:
> SOrthoClub posted: “Summarized by : Dr. Hani Alhebshi An orthodontist can > face cases of dental trauma at his\her practice from time to time. These > traumatic injuries differ in their types, severity and management. This is > a summary of the most common situations of dental tr” >
LikeLiked by 1 person
Informative article. Thank you
LikeLiked by 1 person
Very Informative summary.
Thank you very much Dr. Hani
LikeLiked by 1 person
Most welcome dear Dr. Rwuili
LikeLike
Nice informative topic.
LikeLike